Serious Illness Care
Living Well with Serious Illness and Complex Care Needs
Commonly Asked Questions about MOLST; News About POLST

Serious Illness care is for individuals of any age, from infants to older adults, living with a diagnosed serious illness, advancing frailty and life-limiting medical condition.
A serious illness is often described by clinicians as a health condition or illness, that carries a high risk of mortality (death), and either negatively impacts a person’s daily functioning or quality of life or excessively strains his or her caregivers.
Adults with a serious illness, their Health Care Agents and Guardians, can have a serious illness conversation with their health care providers in order to:
- to better understand their specific health condition and treatment options;
- talk about their goals, values and care choices for the kind of care they want;
- make a treatment plan that honors the individual's goals and care choices.
The Health Care Planning Process below includes important conversations - from simple to serious illness- to make care choices and write down care choices in accompanying planning documents.
Living Well with Serious Illness Starts with a Conversation and a Plan
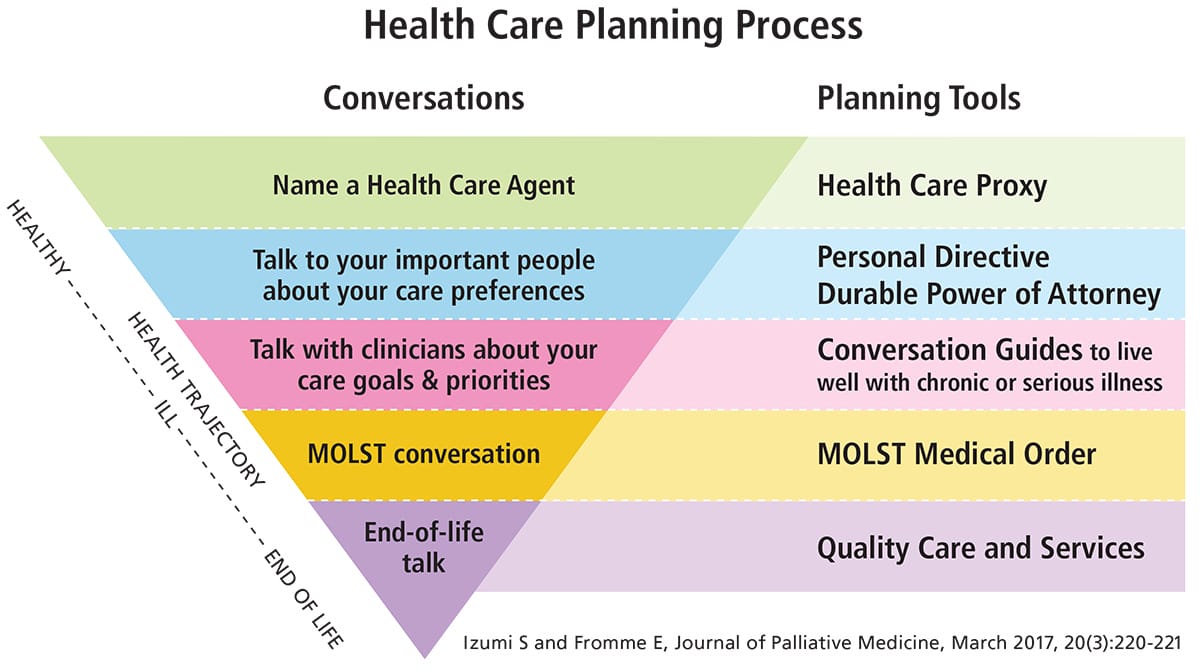
Izumi S and Fromme E, Journal of Palliative Medicine, March 2017, 20(3):220-221
Living well with a serious illness and advancing frailty often starts by making your own personal care plan.
Our Health Care Planning Process (above) makes it easy to have a conversation about the kind of care you want, and write down your care choices in the accompanying planning tools. Your personal care plan helps you talk with your family and your health care providers to get the best possible care that honors your goals, values and care choices, today and everyday over your lifetime.
Make Your Own Plan. Here how it works-
Starting at 18 years old, everyone can use the graphic above to follow the steps in the health care planning process.
- On the left side are the type of conversations that can help you think about and make care choices that are right for you;
- On the right side are the corresponding planning documents to write down your care choices, and guides to help with conversations.
Get Started! The Honoring Choices MA Who's Your Agent? Program® is a easy to use structured approach to care planning. It has tool kits with useful information, conversation guides and planning documents.
- Start a simple conversation to "Name a Health Care Agent", and complete a Health Care Proxy using the Getting Started Tool Kit.
- Then just follow the steps in the process, using the Getting Started and Next Steps Tool Kit, to add and update your plan as your heath needs and choices change over your lifetime.
Everything you need is on the Resources page here.
Let's Talk About MOLST and POLST
Commonly asked questions about MOLST and upgraded POLST Program and Medical Order.
MA MOLST PROGRAM AND MEDICAL ORDER
1.What is MOLST, Medical Orders for Life-Sustaining Treatment?
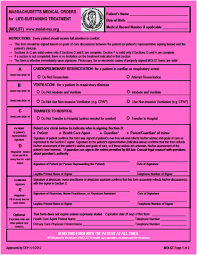
MOLST or Medical Orders for Life-Sustaining Treatment is a medical order that is also part of a broader MOLST Program. The MOLST medical order documents and communicates patient treatment choices and preferences in a medical emergency, if patients can not make or communicate treatment choices themselves. A MOLST medical order helps to ensure patient treatment choices will be known and honored by care providers no matter where the patient receives care.
2. What are life-sustaining treatments?
Life-sustaining treatment refers to medical treatments that are used to prolong life by supporting an essential body function, such as the heart beating, breathing or adequate nutrition, when that body function is not able to work on its own. General, life –sustaining treatment include Cardiopulmonary Resuscitation (CPR), Artificial Ventilation/Breathing, and Artificial Nutrition. Its important to talk with your doctor about your specific medical condition and the risks and benefits of life-sustaining treatment at your stage of health. Whether you choose life-sustaining treatments or not, you will be treated for symptoms and receive comfort care at the end of life. Read more here.
3. Who can use the MOLST Medical Order and how does it work?
MOLST is a medical order designed for individuals living with a serious illness and advancing frailty. As a medical order, it must be completed and signed by a Medical Doctor, Nurse Practitioner and Physician Assistant. MOLST is also considered one of the 5 MA planning documents. Just like all care planning documents, choosing to complete a MOLST medical order with a clinician is VOLUNTARY- it's the patient's choice. Completing a MOLST form should never be a condition for treatment or admission to medical treatment or community facility.
Here’s how MOLST should work:
- The clinician and patient have a serious illness care planning conversation and discuss the patient's medical condition, care goals and treatment options, and the patient's life-sustaining treatment option on the MOLST form;
- The patient make treatment choices for the care they want; the clinician transfers the patient’s treatment preferences to the MOLST medical order and completes the form;
- The MOLST medical order goes into the patient's medical record, and a copy travels with the patient to be followed by all licensed care providers no matter where the patient receives care;
- The clinician and patient/legal regularly review and update the MOLST form to ensure it documents the patient's current care goals and treatment choices.
4. What the status of the MOLST Program?
The MA MOLST Program was first launched in 2010 by the MA Department of Public Health. Unfortunately, the program was never fully developed, and specifically lacks aligned policies and procedures to work smoothly across care and community settings. The MOLST Program lost funding and significant support for education and training in 2014, and has not be updated since that time. As a result, our current MOLST Program is often dysfunction in working across care, community and court settings. The current MOLST program is not fully inclusive of the health needs and rights of historically marginalized populations, adults with complex care needs, and adults under guardianship.
5. What is the Honoring Choices Serious Illness Care- MOLST Challenge?
For the last 10 years the Honoring Choices Partners have been working collaboratively to improve serious illness care and update the MOLST Program. Our Challenge is to build an effective program that is responsive to the changing health needs and care decisions of each individual with advancing serious illness and frailty. A sustainable MOLST Program should center around routine care conversations, supported by key implementation components, to deliver timely, equitable high quality care. We are making steady progress- see the Timeline below.
Great News. POLST is coming to Massachusetts!
MA POLST PROGRAM AND MEDICAL ORDER
1. What is POLST?
POLST, Portable Medical Orders, aims to support individuals with progressive serious illness and advancing frailty engage in care planning conversations with their clinicians and care teams to ensure an individual’s treatment preferences are known and honored.
POLST comes to us from National POLST, a 45- state member organization that develops national standards and an evidence-based POLST process to help states design an effective, sustainable POLST Program. In 2018, Governor Baker announced Massachusetts would join National POLST to upgrade and improve our MOLST process. Currently the MA Executive Office of Elder Affairs is taking exciting steps to transition the state from a MOLST Program to a improved POLST Program. Read more about National POLST here.
2. What would an improved MA POLST Program look like?
The mission of a POLST Program aims to build a responsive process for adults with advancing serious illness and frailty, to respectfully engage in health care planning conversations to understand what matters to each individual, and to ensure an individual's treatment preferences and health care decisions are honoring throughout their illness and at the end of life.
In adopting the National POLST Program, we can upgrade the MA POLST to ideally include-
- an improved process for effective clinician-patient/legal advocate planning conversations
- an improved National POLST medical order/form
- an e-POLST, an electronic POLST medical order completion process
- an electronic statewide registry to ensure POLST orders are accessible 24/7 statewide
Importantly and for the first time, by adopting the National POLST Program, our key program components may include-
- consumer information, multilingual tools & discussion guides
- on-line professional training for health providers and care teams
- critical alignment of equitable policies and regulations across care settings
- a governance structure and statewide stakeholder engagement group
- quality assurance and evaluation process to make improvements
3. How will upgrading to POLST meet the Serious Illness Care- MOLST Challenge?
Transitioning from MOLST to the National POLST Program will help us directly address our deep seated challenges and re-focus our process to help ensure the following:
- The patient/legal advocate and health care provider conversations are at the center of the program;
- The patient/legal advocates can direct their care choices in a personal care plan, which can include a POLST form;
- Build a responsive system where clinicians and care teams can offer timely care and services to honor treatment choices and healthcare decisions.
4. How can you share your experiences and expertise to help build a responsive POLST Program?
The state is currently building a transparent process that welcomes stakeholder engagement to understand our deep challenges and how best to operationalize a new POLST Program. The MA Coalition for Serious Illness Care (MCSIC) is working closely with the State to help transition to the POLST Program. MCSIC sponsors the MOLST to POLST Advisory Group; Ellen DiPaola, Honoring Choices, Erik Fromme, MD are co-chairs, working with Jane Kavanagh, MCSIC. Read more here and share you ideas.
The Honoring Choices community- both consumers and care providers- can lend their voices to inform and guide an upgraded, equitable POLST program. We will get back to you shortly with specific ways to share your knowledge and join an advisory workgroup-
- Consumer Health Equity Advisory Group- Elevating consumer voices to inform and guide policy and program change.
- Guardianship- Serious Illness MOLST Advisory Group- Improving systems to protect the rights of adults under guardianship and ensure timely equitable care.
- Community Serious Illness and Complex Care Need Infrastructure Advisory Group. Shifting the paradigm to build a person-driven, community centered, highly collaborative network of care and services.
Let's inform and guide the POLST Program
It's a timely moment to share your knowledge and lived experiences in order to build an effective upgrade to the MOLST Program. Please send your feedback to inform and guide the new POLST Program. Tell us what you need in your community to correct the problems of the MOLST Program, and build in policies and procedures that are more responsive and inclusive of your populations and support health care and community professionals.
Important Milestones for a Collaborative Serious illness Care Process
Honoring Choices is grateful to be working alongside key leaders to improve the serious illness care for all, and works toward an effective and responsive POLST Program. Here's our progress to date.
2023
March
Honoring Choices launches Community-based Serious Illness and Complex Care Needs Advisory Group
The Covid-19 pandemic spotlighted the structural and institutional racism and discrimination, and inequitable policy and programs in helping vulnerable and underserved adults access essential care in their community. Some of the Honoring Choices Partners got together and invited other like-minded stakeholders to work together to shift the paradigm from a hierarchical infrastructure to an improved community based infrastructure to help individuals live well with serious illness and complex care needs. Our goal is to build a person driven, community centered, highly collaborative network of home and community based care for timely, equitable, high quality care in the community. More information coming shortly.
2022
November
Governor Baker signs Bill to Authorize the State to Build a POLST Program and Registry
Governor Baker signed a Bill H.5374 “An Act Relating to Economic Growth and Relief for the Commonwealth,” that authorizes the Executive Office of Elder Affairs to lead the POLST Program upgrade, by adopting the National POLST model and building a MA POLST Program and registry. The State POLST team has made stakeholder engagement a top priority. The MA Coalition for Serious Illness Care’s MOLST to POLST Advisory Group will develop messaging, tools and training to ensure consumers and care providers have effective care planning conversations to know and honor patient choices in any care setting. The Honoring Choices Partners, working on the "Serious illness care and MOLST Challenge" since 2013,will continue to inform and guide the process.
June
Guardianship Serious Illness MOLST/POLST Advisory Group
The Guardianship Serious Illness MOLST-POLST Advisory Group, co-hosted by Honoring Choices MA and Massachusetts Health and Hospital Associations, continues to work diligently with medical, legal and disability stakeholders to find collaborative solutions to improve due process protections and timely equable care for seriously ill adults under guardianship, The Advisory Group authorized a small working group to specifically examine approaches to improve end of life care matters. The group is also working on a common glossary of terms and definitions that medical, legal and consumers can rely on to understand the guardianship process.
January
MOLST to POLST Transition Advisory Group
The MOLST to POLST Transition Advisory Group is hosted by MA Coalition for Serious Illness Care, working in conjunction with MA Executive Office of Elder Affair's POLST Transition Team to bring the POLST Program to Massachusetts. We are so fortunate to have the expertise of Erik Fromme, MD, Ariadne Labs, lending both his clinical experience and technical National POLST Program skills, to help us implement an effective POLST program at the state level. The Advisory Group is made up of key health care and community stakeholders from health care systems and community programs across the state. The stakeholders work to advise the state on program messaging, program design and development, and vital program implementation components. We are working towards developing a robust education and professional training component in the coming year. The Advisory Group planning team- Anna Gosline and Jane Kavanagh, Massachusetts Coalition for Serious Illness Care. and co-chairs Dr. Fromme, Ariadne Labs and Ellen DiPaola, JD, President, Honoring Choices- are working to build an effective, equitable, and sustainable POLST Program. Read more here.
2021
OCTOBER
UPDATE: MA e-MOLST Web Portal
The eMOLST Web Portal is now closed. The web portal was built as a temporary measure in response to the COVID-19 State of Emergency, when is was not possible to have in person clinician-patient proactive conversations and create a MOLST document. In accordance with State guidelines all eMOLST and MOLST paper documents created during the State of Emergency are valid.
We want to thank everyone for the support of the web portal.
Anna Gosline and Jane Kavanagh, Massachusetts Coalition for Serious Illness Care
Erik Fromme, Ariadne Labs and MOLST to POLST Advisory Group Co-Chair
Ellen DiPaola, Honoring Choices Massachusetts and MOLST to POLST Advisory Group Co-Chair
MAY
UPDATE: MOLST Form and Written Verbal Consent
During the early days of the State of Emergency, in March 2020, we requested the State to allow Witnessed Verbal Consent on a MOLST form, when written in person consent is not possible. The State approved for the duration of the State of Emergency from April 3 to May 11, 2021. Written Verbal Consent also applied to the eMOLST Web Portal Program.
IMPORTANT UPDATE: As of May 11, 2021, MA EMS protocols state the standard for a written signature by patients, Health Care Agents and Guardians on the MOLST form has been reinstated and verbal consent that was allowed during the State of Emergency is no longer accepted, except if the patient is in a licensed care facility. Read more here. EMS can assume MOLST forms completed with patient verbal consent from April 3, 2020 to May 11, 2021 are valid.
2020
OCTOBER
MA e-MOLST Web Portal
The MA e-MOLST Web Portal offers health care providers and seriously ill, high risk and frail adults an effective communication approach to engage in proactive care planning conversations and document patient care choices. The web portal provides easy access to Ariadne Labs Serious Illness Conversation Guides, an electronic MA MOLST form (Medical Orders for Life-Sustaining Treatment), and links to complete a multi-lingual MA Health Care Proxy. The Massachusetts e-MOLST Web Portal is a joint pilot project of the Massachusetts Coalition for Serious Illness Care, Ariadne Labs and Honoring Choices Massachusetts with support from Vynca, Inc.
• Start a serious illness conversation and understand what matter's most
- Download Ariadne Labs Serious Illness Conversation Guides
• Document patient care choices in a MA MOLST form
- If the patient chooses, complete the e-MOLST form in the web portal (English only)
- Alternatively, download and complete a multi-lingual MOLST form, and upload to the web portal
• Simply ask: "Do you have a Health Care Agent?"
- If yes, check that a valid, up to date Health Care Proxy is in the patient record
- If no, download and complete a multi-lingual Honoring Choices Health Care Proxy
APRIL
Helping Adults Under Guaridanship Get Timely, High Quality Care

Guardians are appointed by the court to safeguard an incapacitated person's rights and to make health care decisions to ensure they receive the best possible care. For high risk and seriously ill adults, Guardian's must schedule a court hearing to get approval to make life-sustaining treatment decisions and sign a MOLST( Medical Orders for Life-Sustaining Treatment) form.
For high-risk adult patients with a presumptive or confirmed COVID-19 diagnosis, our physicians report that time is of the essence to clarify care goals and talk about treatment decisions. It can often be a matter of a few hours, or at most a few days, in which physicians and Guardians must make critical decisions to deliver vital care. While the court has made every effort to provide emergency court hearings during the pandemic, we understand Guardians are struggling and additional remedies are needed to ensure every adult receives the best possible care and is not subject to unnecessary harm and suffering.
We respectfully asked the Probate & Family Court to allow Emergency hearing within 24-72 hours to ensure due process and timely, equitable care for seriously ill adults under guardianship.
Additionhally, The Hon. Chief Justice Casey, Probate & Family Court, has generously agreed to join medical, legal and community stakeholders for a first ever Roundtable Discussion to address the guardianship process. Co-hosted by MHA and Honoring Choices. Rescheduled date TBA.
APRIL
Completing a MOLST with Witnessed Verbal Consent
BIG NEWS: As of April 3, and for duration of the COVID-19 State of Emergency, the state has suspended the standard requirement of a written signature on a MOLST form (Medical Orders for Life-Sustaining treatment), and allows for verbal consent to be documented on the form. Verbal consent has been written into the EMS Protocols and will be reliably honored by all EMS personnel and licensed practitioners in hospitals, long-term care facilities and across all health care settings. This offers an important remedy for clinicians and patients where face-to-face MOLST conversations are not possible.
Clinicians can now initiate a proactive planning conversation with patients who are seriously ill or at high risk high risk if they contract COVID-19. Clinicians can speak with competent patients, their Health Care Agents and Guardians, via telephonic or virtual means to discuss goals of care and complete or revise a MOLST form with verbal consent. A copy to MOLST is send to the patient or advocates. See EMS Protocols below for instructions on how to document verbal consent on the MOLST form.
Adults who are considered high risk, their Health Care Agents and Guardians, can call their doctor or treating clinician and ask to have a care planning conversation. The clinician can talk about your medical condition and prognosis, review the benefits and risks of treatment options in the event of COVID-19, and make a recommendation given your personal values, goals and care choices. The clinician will document your care choices on the MOLST form and send you a copy. You can carry your MOLST with you in the event of hospitalization.
Special thanks to Lachlan Forrow, MD and members of our committed MA MOLST and Guardianship-MOLST Advisory Group in sending a letter to the state to request a change in protocols. Read the more here.
Read Emergency Update to the EMS Protocol 7.3 for how to document verbal consent on a MOLST.
MARCH
FInding Two Witnesses to Complete Your Health Care Proxy
During the pandemic, it has become difficult, if not impossible, to have two witnesses physically present to sign Health Care Proxy. So what can you do? To start, remember that competent adults, 18 years old & older, have a civil right to direct their care decisions and to choose an Health Care Agent in a MA Health Care Proxy. If witnesses are not available during this State of Emergency, you can use the MA Health Care Proxy to create a personal document to choose a Health Care Agent. Although not a legal document, your personal document is evidence of who you want to be your trusted decision-maker and should be respected by your family and your physicians.
Here's how to create a personal document:
- Download the MA Health Care Proxy. This document is recognized in MA as the means to communicate your choices;
- Fill in information and sign the document;
- In the Witnesses section, write in: "Witnesses not available during the COVID-19 State of Emergency";
- Give copies to your Agent, family, and physicians;
- After the State of Emergency is lifted, you can update your Health Care Proxy and sign in front of two witnesses to create a legal document.
- Complete your Personal Directive. Tell your Agent what you want for care.
- If you are at high risk for COVID-19, you can call your primary care physician to talk about your medical condition and the benefits and risks of treatment decisions. Fill out your Personal Directive, and if you like, complete a MOLST form with your clinician.
FEBRUARY
UPDATE: MA Adopting National POLST & Process

I am delighted to share that the Executive Office of Health and Human Services (EOHHS) informed the DPH MA MOLST Advisory Subcommittee that they received the Subcommittee’s recommendation to adopt the National POLST form and process for use in Massachusetts, and as a result, is in process of developing a multi-year plan to move from MA MOLST to National POLST.
We are excited to join National POLST , a 43-state movement that has adopted a national standard of care for adults with serious illness. With their deep expertise and evidence-based materials, we can build an improved collaborative process that delivers quality person-directed care to adults with serious illness from first diagnosis, through managing treatments, to end of life. For the present, our MA MOLST form and process remains in place as the next phase begins to build a multi-year plan.
I join EOHHS in thanking the members of the MOLST Subcommittee for their invaluable work over the last two years, with guidance from the DPH Palliative Care & Quality of Life Interdisciplinary Advisory Council. I’d also like to thank the Guardianship-MOLST Advisory Committee, co-sponsored by Honoring Choices MA and MA Health & Hospital Association, working in tandem with the Subcommittee to safeguard the rights of individuals with serious illness under guardianship.
Additionally, my deepest gratitude to the hundreds of Honoring Choices Partners who sparked this process with the 2017 "MOLST Meeting the Challenge" statewide tour, and who have contributed to "Important Milestones" on this journey. Your first-hand knowledge of the real life challenges adults and families face, and suggestions for collaborative solutions, has been essential to the success of the MOLST Advisory Subcommittee's work.
We have received many questions about next steps, and dozens of offers to help contribute to the process. We have made note of all and thank you for your continued commitment and generosity. We'll keep you posted and look forward to engaging all your expertise in the next phase of implementation.
Ellen M. DiPaola, Esq. Chair, DPH MOLST Advisory Subcommittee
President & CEO, Honoring Choices MA
NOVEMBER
Excitng Progress: UPDATE on Improving the Serious Illness Care and MOLST Process

The MA MOLST Advisory Committee has put together a one-page update of major milestones this year and exciting next steps.
Read about the progress to come into compliance with the National POLST standard and improve our Serious Illness Care and MOLST process!
2019
OCTOBER
We are "In the Pink"!
National POLST has upgraded Massachusetts from "unaffiliated" to "active" status on its national map of state programs. That's a significant leap and recognizes the collaborative work to date to improve our MOLST form and process and come into compliance with the national POLST standard. It's a moment to thank the many state leaders, health care and community experts who have paved the way here. We stand on your shoulders and will respectfully build on your work. Read more about our rich history and current achievements in the "Important Milestones " timeline below.
See the POLST State Map here
SEPTEMBER
DPH MA MOLST Advisory Committee recommends adoption of the national form

The 28 member MA MOLST Advisory Committee, a subcommittee of the Department of Public Health (DPH) Palliative Care & Quality of Life Interdisciplinary Advisory Council, has completed a comprehensive review of our rich history and our current problematic, often dysfunctional MOLST process. The MA MOLST Advisory Committee voted to recommend to DPH that we adopt the national form and process for use in Massachusetts, to be accompanied by a MA Implementation Guide that reflects our improved governing structure and key implementation components.
Once the new form is adopted, the Advisory Committee can get right to work on the implementation process to include:
- build-in a governing structure with professional training, consumer education, and quality control;
- align protocols & procedures under the new form across all health care, community & court settings;
- create a simple MA Implementation Guide.
Next Steps: The Department of Public Health is reviewing the MA MOLST Advisory Committee’s recommendation and will make a determination of adopting the national form and process shortly.
Read more- "A Game Changer for Living Well with Serious Illness" here
SEPTEMBER
Just released: First National POLST form
The National POLST Paradigm announced the release of the first national POLST form and accompanying materials. Representatives of the 43-state POLST collective worked together to create the new form. The MA MOLST Advisory Committee contributed to several drafts of the new form, including the new and improved treatment decision sections. The national form will now be adopted by individual states. It's an exiting milestone for the country and will strengthen our national standard of care, create reciprocity across state lines, and provide states with standardized evidence-based tools, and key implementation components such as professional educational training, consumer education material, quality monitoring systems and much more. Next Step: the DPH MA MOLST Advisory Committee will re-convene to vote on possible adoption of the national form for use in Massachusetts.
Read more- "A Game Changer for Living Well with Serious Illness" here
JUNE
NEW EMS Protocols : Authority of the Health Care Agent and others

There are two important changes to the Emergency Medical Services (EMS) Statewide Treatment Protocol 7.3 Medical Orders for Life Sustaining Treatment (MOLST) and Comfort Care/Do Not Resuscitate (DNR) Order Verification (CC/DNR:
- To provide for an exception allowing for box D of the MOLST form to be signed by an alternate person for patients located in the licensed health care facility. The health care facility assumes full responsibility for this signature documenting the authorization of the activated health care agent or guardian. EMS can assume the form is valid in these cases.
- To add a provision reflecting a health care agent’s and guardian’s legal authority under law, that no matter where EMS encounters a patient, if the patient’s lacks capacity/competency and the patient’s health care agent or guardian is on scene with his/her legal authorizing document in hand, the health care agent may change or revoke the patient’s existing MOLST form instructions.
The full protocols are posted at : https://www.mass.gov/lists/emergency-medical-services-statewide-treatment-protocols.
National POLST Education Committee meets to designs tools to share with all states

Ellen DiPaola, Esquire, a member of the National POLST Paradigm's Education Committee and Honoring Choices President & CEO, is working with multi-disciplinary care providers from across the country to build a more robust POLST/MOLST serious illness education program at a national level. The Education Committee will design a comprehensive program to include-
• A standardized set of free fact sheets, videos, webinars available to all MA patients and providers;
• Post serious illness resources from 45 states to share best practices and programs;
View and download the current National POLST Paradigm tools here.
JUNE
MA MOLST Advisory Committee contributes to the new National POLST form
The National POLST Paradigm had an inspired idea .... to create one National POLST form, instead of 45 separate state forms, and set a national standard to understand and honor patient's care choices. Our 28 member MA MOLST Advisory Committee has been working diligently to contribute edits to several drafts of the proposed National POLST form. The final form is due in early September 2019. The MA MOLST Advisory Group will re-convene to review the final version and suggest next steps to the state. If adopted by Massachusetts, the new form will help to standardize and greatly improve our MOLST process for all stakeholders. The new national form will come with informational guides, evidence-based professional training resources and consumer educational materials. Keep you posted.
MAY
MA delgates attend the first National POLST Plenary Assembly Summit

Christine Michael, MA delegate to the National POLST Plenary Assembly and Executive Director of Hospice & Palliative Care Federation of MA, helped organize and attend the first national meeting of delegates from 45 states in Austin Texas. The Plenary Assembly set to work on crafting a national standard and national POLST form, being inclusive of their state specific issues and evidenced based objectives. Christine McMichael and Ellen DiPaola, Esq, President & CEO, Honoring Choices are the two MA delegates to the National POLST Plenary Assembly. They are working to bring evidenced-based programs and best practices to the Commonwealth.
NEW: Introduction to Guardianship Training for family members and guardians

The Massachusetts Guardianship Policy Institute established the Massachusetts Guardianship Academy to provide education, training, and support to guardians, volunteers, family and those in need of advance directives. The Academy has programs on the basics of guardianship; how to be a guardian; how to be a health care proxy and; the importance of advance directives. The Academy’s first trainings were for professional and lay guardians. In June 2019 the Academy began providing an Introduction to Guardianship Training to family members and recently appointed guardians in conjunction with the Volunteer Lawyers Project at the Suffolk Probate and Family Court. Training for the Plymouth Probate and Family Court Volunteer Lawyers Program began in September 2019. In October 2019 the Academy provided its first Introduction to Guardianship Training in Spanish that included an interpreter and translated materials at the Suffolk Probate and Family Court location. The Academy regularly hosts Guardianship Rounds to discuss where a complex guardianship cases. Future plans include providing additional language specific training for Probate and Family Courts in the Commonwealth as well online training modules and live streaming of educational events. For more information contact Traci Cucinotta, MBE, MSW, LICSW , Education and Training Specialist, Guardian Community Trust, 978.775.3500.
JANUARY
DPH AdvisoryCouncil recommends New MOLST Governing Structure and Key Program Components
We are on our way! The MA MOLST Advisory Committee provided it's "MA MOLST Program Key Elements & Standards Report" to the full DPH Advisory Council, which voted unanimously to recommend the report's adoption to the state. Lachlan Forrow, MD, DPH Advisory Council Chair (pictured here) made the official recommendation to Dr. Elizabeth Chen, then Associate DPH Commissioner, who responded favorable. It gives the MA MOLST Advisory Committee the green light to build an improved Serious Illness and MA MOLST Program governing structure to include key program elements such as:
• New MOLST form and process compliant with national standard;
• Unified regulations, policies & procedures for all stakeholders;
• Professional training and consumer education programs;
• Quality control and monitoring component.
2018
DECEMBER
Honoring Choices and MHA co-convene Guardianship-MOLST Advisory Group

• "Does a Guardian have the authority to sign a MOLST form?"
• "Does a family member of an incapacitated person (not a Health Care Agent or Guardian) in agreement with the treating physician's care plan, have the authority to make end of life care decisions?"
• "How does the court process empower Guardians to work with treating clinicians at first diagnosis through to end of life care, just as Health Care Agents do, to ensure the incapacitated adult receives timely quality care?"
These are just a few of the complex questions Honoring Choices Partners, hospital personnel and attorneys face everyday. We hear increased reports of incapacitated persons are being treated as "second class citizens" and experiencing inequitable care and unnecessary harm and suffering. To understand the issue and find solutions, Honoring Choices and the Massachusetts Health and Hospital Association have co-convened a 20 member Guardianship-MOLST Advisory Group. We hope to work with the Probate and Family Court to clarify the role of a Guardian in serious illness, and align the court's protocols and procedures with other key stakeholders such as hospitals, skilled nursing facilities, hospice and EMS protocols. Together we can work to ensure the incapacitated adult will have the same quality and timely care as adults with capacity.
View a list of the Guardianship-MOLST Advisory Group members.
JUNE
The 28-member MOLST Advisory Committee gets to work!

The MA MOLST Advisory Committee expanded to bring in the expertise of a multi-disciplined health care providers and community professionals who represent a wide diversity of adults across the Commonwealth. Our charge from the MA Dept of Public Health is to help Massachusetts come into compliance with National POLST Paradigm standard, and to create a conversation-based, team approach process to help stakeholders across all care settings know and honor an adult's choices for care.
MAY
New Guide- "EMS & MOLST: 5 Things You Can Do Ahead of an Emergency"
The 5 MA Emergency Medical Services (EMS) Regional Directors worked closely with Honoring Choices to create 5 important things we can all do to help ensure a medical order is valid, visible and can be honored in a medical emergency.
Many thanks to 5 Regional EMS Directors who spoke with hundreds of care providers across the Commonwealth on the HCM MOLST Challenge Tour, in order to create this simple guide for high quality, smoother care transitions. The guide is posted on the Honoring Choices website.
FEBRUARY
NEW Tools: Honoring Choices introduces Palliative Care Discussion Guides
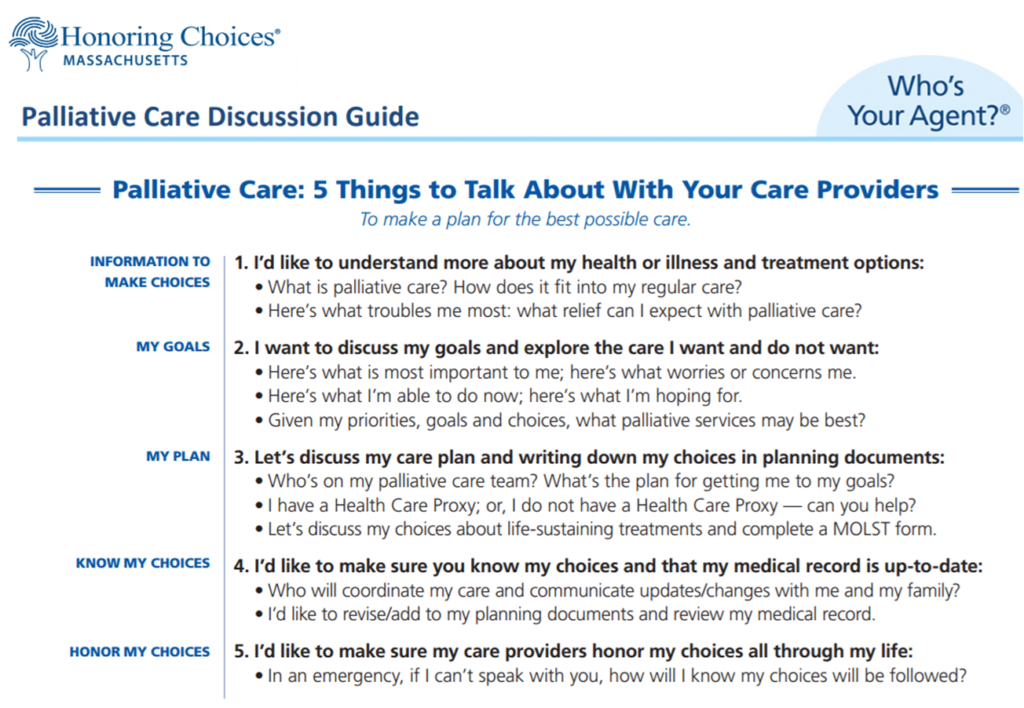
Doctors and care providers consistently agree starting a "MOLST discussion" with a patient at first diagnosis is a "best practice." The discussion allows patients to: 1. Understand their prognosis and treatment options to create goals of care; 2. make choices about life-sustaining treatments; and 3. explore palliative care to manage the pain, symptoms and stress of serious illness. Honoring Choices is pleased to offer our new Palliative Care webpage with two free, downloadable discussion guides:
• "5 Things To Talk About With Your Care Providers"; a handy guide for consumers; and
•"5 Things To Talk About With Your Patients & Clients"; a handy guide for providers.
Read More about Palliative Care Discussion Guides here.
2017
JUNE
The Probate & Family Court: A Key Stakeholder in the MOLST Process

On June 8, Honoring Choices was invited to Guardianship Committee of the Probate and Family Court, to provide a update on MOLST. Ellen M. DiPaola, Esq., President & CEO, provided a status report to the Guardianship Committee's Judges and Assistant Judicial Case Managers who oversee guardianship petitions and a guardian's request for permission to sign a MOLST form. The court is considered "a major stakeholder" in helping to safeguard and improve the serious illness journey for an incapacitated person, and to support a Guardian's role/responsibility to protect the rights of an incapacitated person and provide for essential care. We had a thoughtful discussion regarding the opportunity to improve the MOLST form, and align court protocols and procedures with fellow medical and community care stakeholders. We agreed an Honoring Choices Work Group will be formed to explore the Committee's suggestions and report back for further discussion.
JUNE
Govenor Baker's office announces MA to Join the National POLST Paradigm

The Massachusetts Department of Public Health, who oversees the MOLST process, is taking steps to join the national patient-directed serious illness initiative. The National POLST Paradigm was established in 2004 to establish national quality standards for POLST / MOLST Paradigm Programs, and to assist states in developing their programs. They have a extensive website of evidence based research, webinars, tool kits and more. Joining National POLST will offer Massachusetts a well-established, evidence based model to consider for crafting our state program. Secretary Alice Bonner, MA Executive Office of Elder Affairs announced the news at the May 9 MA Coalition for Serious Illness Care's Annual Meeting.
Read more about National POLST Paradigm
To Access Tool Kits and Webinars. Click Here
MAY
Honoring Choices kicks-off the "MOLST Meeting the Challenge Tour"

Over 100 multi-disciplined care providers and professionals came together for the first-ever unique forum to hear a dynamic panel discussion and lend their expertise to crafting a more responsive and aligned MOLST process. The Massachusetts Medical Society co-hosted our inaugural Metrowest-Boston and North Shore Workshop to open a state-wide dialogue about understanding the complex issues and building a better process. The MOLST Challenge Tour will host workshops in all of the 6 Honoring Choices Regional Networks. Each workshop assembles a panel of local experts including the regional EMS Director.
APRIL-DECEMBER
Cape Cod Hospital hosts "MOLST: Meeting the Challenge Workshop"
Our second in the series of MOLST Workshops took place at Cape Cod Hospital with a diverse group of care providers from its 62 Member Task Force to discuss both statewide and regional challenges. The panel members and care providers focused on the unique challenge of crafting a coordinated regional response Cape-wide for assisting a large year-round elder population and seasonal residents who may not have their medical documents in-hand. Each task force member represents a local care setting on the Cape. Together they are a dynamic movement for crafting sustainable change for a responsive MOLST process in their region. "Outcomes Report" to follow.
Baystate Health hosts Holyoke/ Springfield's "MOLST: Meeting the Challenge Workshop"
Care providers in the Holyoke, Springfield and Western Massachusetts regions attended the MOLST: Meeting the Challenge Workshop at the Baystate Health Education Center, 361 Whitney Avenue, Holyoke. The third in our series of MOLST Workshops was generously hosted by Honoring Choices Alliance Partner, Western MA Transitions in Care Cross Continuum, sponsored by Baystate Health.
UMass Memorial Medical Center hosts Worcester. MOLST: Meeting the Challenge Workshop
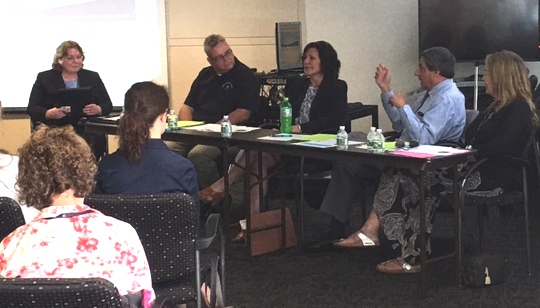
All care providers in the Worcester and Central Massachusetts region came together to exchange ideas with this dynamic panel (pictured here), for a MOLST: Meeting the Challenge Workshop at the First Unitarian Church of Worcester. This is the fourth in our series of MOLST Workshops.
Hawthrone Medical Center hosts South Shore MOLST: Meeting the Challenge Workshop

Over 65 interdisciplinary care providers from the Dartmouth, New Bedford, Fall River and and South Shore region attended the MOLST: Meeting the Challenge Workshop at the Hawthorne Medical Center, Dartmouth. This is the fifth in the series of MOLST Workshops.
2016 November
MA Coalition for Serious Illness Care

The mission of the Massachusetts Coalition for Serious Illness Care (Coalition) is to ensure that health care for everyone in Massachusetts is in accordance with their goals, values, and preferences at all stages of life and in all steps of their care. The Coalition has established six core priorities including: naming a Health Care Agent; talking with your agent, family, and providers about care goals, values, and choices; providing the necessary training for clinicians; and building effective systems to ensure individual preferences and choices can be documented, shared, and honored in every care setting. More than ninety Massachusetts-based organizations form the Coalition and are working on shared goals to support the Coalition’s mission. In 2016, the Coalition fielded the first of a regular series of surveys measuring Massachusetts residents’ views on serious illness and end-of-life care. The Coalition hosts an annual spring summit each year open to all. Learn more, and become a member.
2008-2014
Rich History of MOLST Implemenation
Many hundreds of professionals have brought us to where we are today. They were and still are the guiding stewards of this process and we gratefully stand on their shoulders to continue their work. The MA MOLST website has the following summary of our rich and deep history.
2008 - MA legislature enacts Chapter 305 of the Acts of 2008, Sections 41–43 to require the establishment of a MA MOLST demonstration program in at least one area of the Commonwealth.
2009 - MOLST Demonstration planning begins. The greater Worcester area is selected for the demonstration due to its size, number and diversity of health care providers, and ongoing community-based efforts to improve end of life care.
2010 - In February, MA DPH Circular Letter: DHCQ 10-02-529 supports MOLST use to meet the “standard of care for communicating patient preferences regarding life-sustaining treatment options.”
2010 - In April, the MOLST Demonstration program is implemented involving two acute care hospitals; five skilled nursing facilities, home health and hospice providers; one primary care home-visiting program; and regional emergency medical services.
2010 - The Massachusetts Expert Panel on End-of-Life Care Report recommends that "full statewide implementation of MOLST should be achieved no later than January 1, 2014."
2011 - MOLST Demonstration Report recommends statewide expansion of MOLST, stating that, "as a result of the overwhelmingly positive findings from the MOLST Demonstration Program, the MOLST Steering Committee holds the vision that in Massachusetts: 1. Every suitable patient will be offered the opportunity to utilize a MOLST form in concert with that patient’s clinician to communicate life sustaining treatment preferences across health care settings; 2. Every emergency medical technician will receive MOLST training and be authorized to honor valid MOLST forms; 3. Every major hospital system and health care plan will implement policies and procedures to facilitate the appropriate utilization of MOLST by clinicians and patients; 4. Every clinician will seek to improve communications skills with patients nearing the end of life; have access to MOLST education; and be encouraged by professional organizations and regulatory bodies (e.g. Boards of Registration, Massachusetts Medical Society) to utilize MOLST correctly; and 5. MOLST forms as well as education and outreach materials will be uniform; linguistically appropriate; culturally relevant; easily available; accessible to persons with disabilities; and recognized by health professionals and consumers alike."
2012 - MOLST statewide expansion announced in MA DPH Circular Letter: DHCQ 12-3-560 and statewide expansion of MOLST use begins.
2012- The MOLST Committee provides education, support and professional training.
2014 - MOLST form in use in clinical care institutions statewide. Read the April 2014 report, MOLST Statewide Expansion Evaluation Findings.
2014- The MOLST Committee is disbanded. Effective July 1, 2014 the MOLST Project will transition to the MA Department of Public Health.