Conversations on the Rise: Weaving ACP Billing Codes Into Your Practice for Multiple Advantages
Since January 1, 2016, Centers for Medicare and Medicaid Services (CMS) has provided reimbursement for clinicians to engage patients in advance care planning discussions with the goal of providing improved patient-and family-centered care for Medicare beneficiaries. The two reimbursement codes enable Medicare patients to make informed care decisions to improve healthy aging and to plan for future care.
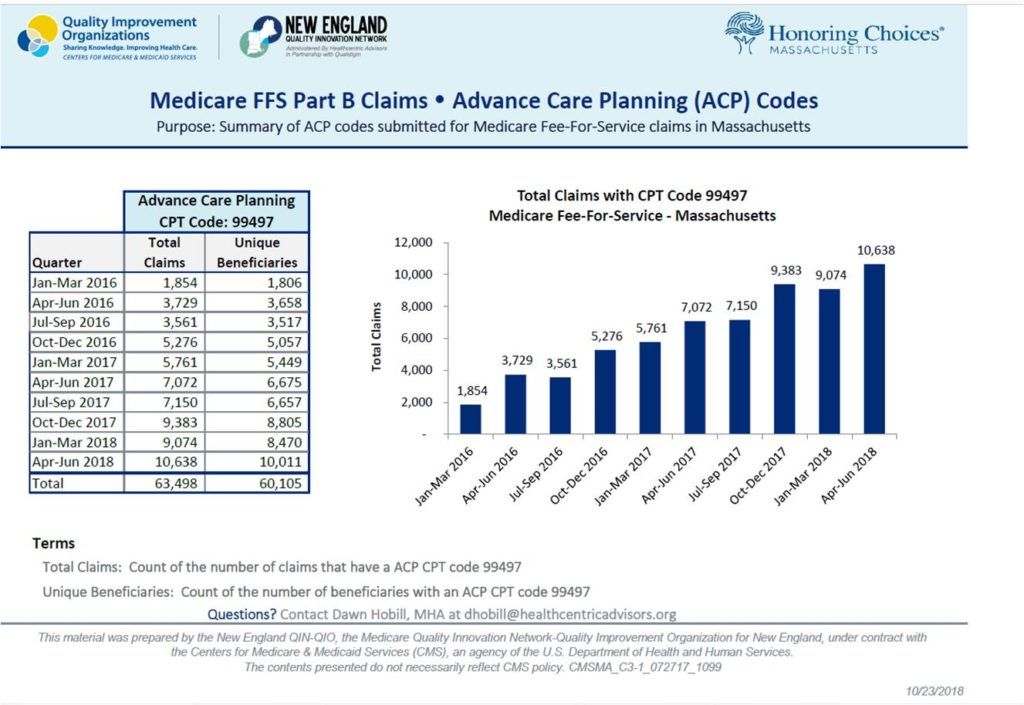
“The data shows there has been a steady increase in the number of Advanced Care Planning conversations billed by physicians in Massachusetts,” says Dawn Hobill, Senior Program Administrator, Healthcentric Advisors. “Medicare Fee for Service Claims indicates between Q1 2016 and Q2 2018, that there was a 474% increase in the number of ACP conversations billed, a hopeful sign that a patients end of life goals and preferences are being discussed and documented with their primary care physician.” Here’s a helpful graphic provided by Healthcentric Advisors.
That’s also great news for Massachusetts consumers who can call their physicians to request an advance care planning appointment. Clinicians across health care settings report they have successfully weaved advance care planning discussions into their daily work flow by scheduling add-on sessions to a regular appointment or a care management session and billing for both. Since physicians and non-physician practitioners may bill, health systems have employed a team approach and trained their staff to routinely engage adults in care planning discussions and complete care planning documents across all care settings.
Additionally, clinicians report that routine ACP discussions foster multiple benefits in advancing and reporting on quality care and coordination measures, including:
- Meeting Accountable Care Organization goals;
- Using a team approach for routine, effective ACP discussions helps providers consistently deliver high quality patient driven care;
- Advancing Quality Improvement Measures for all patients;
- Improving Quality of Life Measures for patients managing chronic illness and living with serious illness.
Working together with Healthcentric Advisors, an Honoring Choices Alliance Partner, here is up to date information on the ACP billing codes, their multiple advantages, and how to embed care planning tools at your practices.
What are the reimbursement codes and how can I use them?
Medicare pays for voluntary advance care planning (ACP) discussions under the Medicare Physician Fee Schedule (PFS) and the Hospital Outpatient Prospective Payment System (OPPS). The reimbursement codes may be used across all care settings and at any phase of health. No specific diagnosis is required. The billable ACP discussions can be provided as often as needed and at the discretion of the patient. Medicare uses two reimbursement codes:
- Code 99497 pays for “ACP, including the explanation and discussion of advanced directives such as standard forms (with completion of such forms, when performed), by the physician or other qualified healthcare professional, first 30 minutes, face-to-face with the patient, family member(s), and/or surrogate”;
- Code 99498 reimburses for each additional 30 minutes. Code 99498 is an add-on code and so can only be used along with code 99497. Read more.
What’s advance care planning and the Massachusetts planning documents?
Advance care planning is not a ‘one off conversation’ or completing one document, but a dynamic process that requires regular and thoughtful discussions between a clinician and patient, their family, Health Care Agent or Guardian. It creates a powerful patient-care provider shared discussion process about a patient’s medical condition and prognosis, the benefits and risk of treatment options, sharing of the patient’s values, beliefs and priorities that impact care choices, and creating care goals to receive quality everyday care and future care. Health care providers can help patients write down their care choices by completing Massachusetts planning documents, such as a:
- Health Care Proxy: Choose a Health Care Agent (Agent) and appoint in a Health Care Proxy;
- Living Will: Give instructions to your Agents and care providers on the kind of care you want and do not want;
- MOLST, Medical Orders for Life-Sustaining Treatment: For patients with serious illness of fraility, a shared clinician-patient discussion about a patient’s current condition, where a patient makes choices about life-sustaining treatments which is recorded by the clinician in a MOLST form.
- CC/DNR, Comfort Care/Do Not Resuscitate Order: For patients with serious illness, a shared clinician-patient discussion about a patient’s current condition, where a patient chooses that medical personnel do not attempt Cardiopulmonary Resuscitation (CPR),but provide comfort care measures.
What are the challenges to adopting the ACP Reimbursement Codes?
Although reimbursement for voluntary ACP discussions is on the rise, there are several barriers and challenges to its full statewide adoption. Read more. Honoring Choices MA Partners,who are multi-disciplined health care and community care providers, have identified the barriers and challenges as follows:
- Physicians and health systems do not know about the codes or have not yet incorporated into their payment system;
- Finding the time to weave in a 30 minute ACP discussions into the busy patient work flow, especially in primary care practices; Read more;
- Lack of trained clinicians and non-clinician staff to confidently engage adults in ACP discussions and help patients’ complete care planning documents.
What are the benefits of early and routine ACP discussions?
“We are seeing the multiple advantages to incorporating advance care planning conversations into the daily workflow for physician and for patients,” says Ms. Hobill, Healthcentric Advisors. Here are four noteworthy advantages:
1. Meeting Accountable Care Organization Goals
According to the CMS, the goal of Accountable Care Organizations (ACOs) is to provide coordinated care “to ensure that patients get the right care at the right time, while avoiding unnecessary duplication of services and preventing medical errors.” To know how to offer patients ‘the right care at the right time’, a clinician must ask each patient about their care goals, values, priorities and care choices, in order to match essential care when the patient needs it, and all through their lifetime. ACP discussions can directly achieve ACO goals to:
- Provide high quality care aligned with patient choices;
- Avoid unnecessary or duplication of medical services;
- Improve quality and safety to prevent medical errors;
- Drive down costs to share in savings within the ACO program.
2. Using a team approach for routine, effective ACP discussions helps providers consistently deliver high quality patient driven care
The ACP reimbursement code guidelines support a team approach to provide advance care planning for every patient in any setting. In a team approach, all clinicians and staff are trained to confidently engage adults in ACP discussions, complete MA documents, and to refer to their team members as needed for clinically-based or in-depth conversations. In a team approach, billing codes can be used as follows:
- By all physicians or qualified health professionals, defined as a non-physician providers, including nurse practitioners, physician assistants, and clinical nurse specialists;
- Members of your healthcare team are reimbursable if performed “incident to” the services of a billing practitioner, including a minimum of direct supervision;
- As an add on session to a routine appointment, wellness visit, or care management visit;
- In all settings, inpatient and outpatient, assisted living, nursing home and home settings.
3. Advancing Quality Improvement Measures for all Patients
Routine advance care planning discussions and knowing a patient’s goals, values and care choices, can directly improve quality improvement measures of patient satisfaction, reducing adverse drug effects, and reducing unnecessary re-admission rates.
Clinicians who are eligible to report to the Quality Payment Program (QPP) in performance year 2018 are required to submit data in order to avoid the 5% negative payment adjustment to their Medicare Part B claims. In performance year 2019, this negative payment adjustment increases to 7%. There are 4 categories included in reporting; Quality, Improvement Activities, Promoting Interoperability, and Cost. You can learn more here.
“Clinicians who are implementing advance care planning into their daily workflow may report on the Quality Measure (ID 047) Care Plan” says Ms. Hobill, “which simply involves identifying the percentage of patients aged 65 years and older who have an advance care plan or surrogate decision maker documented in the medical record that an advance care plan was discussed. CPT codes 99497 and 99498 satisfy the requirement for this measure.”
As well as the quality measure mentioned above, the Improvement Activity IA_PM_21 – Advance Care Planning (see details here . This improvement activity is a medium-weighted activity and would earn a small practice 7.5 total MIPS points and a large practice 3.75 total MIPS points. Note, for performance year 2018, clinicians need to earn at least 15 total MIPS points in order to avoid the negative payment adjustment. In performance year 2019, this performance threshold increases to 30 points.
4. Improving Quality of Life measures for patients with chronic illness and serious illness
ACP discussions are an integral part of managing chronic illness and improving care coordination. The depth and frequency of care planning conversations generally increases over time with patients who are seriously ill or medically frail. Multiple clinician-patient discussions typically include discussing changing health needs and treatment options, Palliative Care, Comfort Care, Hospice Care, and MOLST discussions to complete and update a medical order. It’s important to note ACP reimbursement codes may be billed as often as every day at the patient’s discretion. Having regular discussions help to communicate timely care choices to the care team, coordinate safe care transitions, and ensure patient choices are honored at the end of life. To improve quality of life measures, the ACP codes can be used in conjunction with:
- Chronic care management codes;
- Transitional care management codes;
- Palliative care codes to manage the pain, symptoms & stress of serious illness (Read more);
- Hospice care for patients who have elected the Medicare Hospice Benefit.
How can care providers weave ACP discussions into their workflow?
Honoring Choices MA provides a structured, team based approach to health care planning to help clinicians and all staff confidently engage adults in health care planning conversations. Our free, downloadable “Getting Started Tool Kit” includes:
- MA Health Care Proxy to choose a Health Care Agent;
- MA Personal Directive(Living Will) to give your Agent information and instructions about your care; and,
- “5 Things to Talk About With Your Care Providers” a handy discussion guide to start a goals of care conversation.
Care providers and staff can be trained as “Health Care Planning Ambassadors” to engage adults in powerful yet simple discussions. The Ambassador Manual helps practice managers easily embed the tools kits into their programs to help “Every Patient, Every Visit.” It’s free and easy to use. Contact Ellen, edipaola@honoringchoicesmass.com
Many thanks to Dawn Hobill and our Alliance Partner, Healthcentric Advisors, for working together to bring you this up to date information. Healthcentric Advisors is a national health care quality improvement authority. Since 1994, they have been providing technical assistance, education, and data analysis to health care providers throughout New England and the nation. Healthcentric Advisors as the lead contractor the New England Quality Innovation Network-Quality Improvement Organization (NE QIN-QIO) serves as a centralized resource for knowledge to help providers improve the quality, efficiency and value of healthcare for all Medicare Fee for Service beneficiaries in New England. For more information please visit their website here.